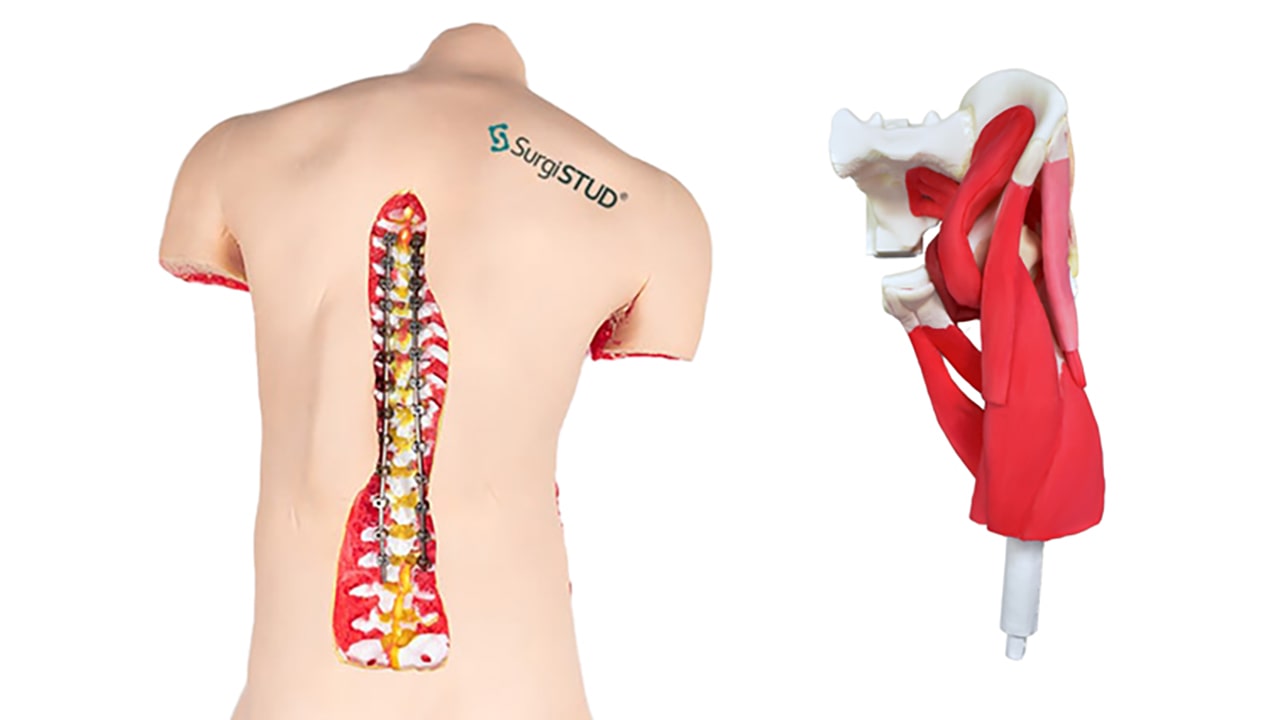
These training models, which eradicate concerns of cadaver supply, screening, and storage, allow medical device companies, orthopedic and spine surgeons, residents and fellows to safely rehearse a multitude of procedures with a range of real-life anatomies and pathologies.
The Spine Experience
“My colleagues and I see some challenging idiopathic scoliosis curves, often greater than 100 degrees,” says Kenneth Illingworth, M.D., an orthopedic surgeon and director of Pediatric Trauma at Cedars-Sinai Hospital in Los Angeles. “One of my charges as the Associate Residency Program Director for Orthopaedics is to provide and advance education. So, when I learned about the SurgiSTUD models, I set out to incorporate them into our surgical simulation training.”

Dr. Illingworth, who has been involved in other teaching models and cadaver labs, states, “The SurgiSTUD model is quite realistic in terms of haptic feedback, the ability to put screws in and use drills, pedicle screws and rods. Importantly, this model offers a truly realistic environment for the trainees to learn how to use this instrumentation around sensitive areas. We worked with SurgiSTUD to develop a severe pediatric spinal deformity model and took some of our residents through this simulation protocol. They rated it as one of the top educational experiences they have ever had.”
The academic publishing world took notice as well. “The Journal of the Pediatric Orthopaedic Society of North America [“Simulation Training in Pedicle Preparation and Screw Insertion in Pediatric Spinal Deformity”] reached out to us to do a paper because they had a special edition on surgical simulation, and they knew of the pediatric spinal deformity work we were doing with SurgiSTUD,” says Dr. Illingworth. “In August 2022, we published our technique in detail as far as how we were training residents prior to them entering the OR.”
Playing With Trajectories, Angles and, Literally, Turning the Model 360o
“The SurgiSTUD static/interactive model was fantastic!” states Dr. Illingworth. “Working with a severe curve, we put interactive dowels on the optimal pedicle trajectory track so that the residents and fellows could ‘play’ with the trajectories and then go straight over to the simulated OR environment with the SurgiSTUD model in order to practice those trajectories.”
“What can be a challenge intraoperatively is that it’s tough to understand the 3D anatomy when you’re just looking at it from the back. So, the static model gives trainees the ability to turn things around 360 degrees, look at the trajectories and how they are changing as the rotation changes through the spine. This means that when surgeons get into the OR they have a better idea of the rotation and angles, as well as where the starting positions are.”
Faster Learning Curves
Taking a cadre of junior-level residents, most of whom had never set foot in a pediatric spinal deformity case, Dr. Illingworth did a post-simulation questionnaire. “At the outset, prior to using the SurgiSTUD model, they were all very uncomfortable with spinal instrumentation and the process. The follow-up questionnaire showed, however, that they gained a significant amount of knowledge and felt much more comfortable going into the OR because they had practiced on SurgiSTUD.”
After this success, he and his colleagues obtained a grant from the San Diego Spine Foundation. “Now we are furthering our study on SurgiSTUD models, comparing the training environment to the actual intraoperative environment in terms of how the residents fare, as well as looking at the safety profile of these techniques.”
“We don’t have cadaver facilities on campus…”
“At Cedars Sinai we don’t have cadaver facilities on campus, so in the past when trainees got hands-on experience at cadaver courses there were several issues. Not only are the cadaver sessions difficult to schedule, but there is a significant amount of cost involved. Also, from a spine perspective, there is a huge variability in the cadaver specimens. You might get a giant specimen where the pedicles are so big that nobody’s going to be able to get any sensation or haptic feedback as to how to put screws in. The cadavers don’t have the necessary scoliotic curves, sometimes the dissection takes up the majority of your time, and sometimes the cadavers are frozen, thus making it difficult to insert instrumentation.”
“Synthetic models eliminate some of those variables and allow you to actually focus on the education element of the process. It also allows us to train on different pathologies. As a complex spinal deformity surgeon in pediatrics, I am rarely operating on a straight spine. If we have a cadaver with a straight spine, it’s very hard to teach someone how to drop their hand on a 100-degree curve where they are literally putting a screw in parallel to the floor. But you can do that on synthetic models. You can take any of your patients or any severe curvature, print out these models and train on them.”
Regarding how SurgiSTUD compares to a bone or a cadaver, Dr. Illingworth points to the extreme variability in cadavers in terms of bone density and bone size. “In cadavers, there is too much variation as far as how the haptic feedback and instrumentation correlates to what we do in the OR. The ability to control all the variables with synthetic models is truly valuable.”
“In my experience, using the SurgiSTUD models really gave me quite realistic haptic feedback in terms of instrumenting pedicles. You can feel the pedicle walls…it felt very genuine compared to the intraoperative environment. If you had a pedicle breach medially or laterally secondary to the soft tissue that encases that portion of the bone, you could get good tactile feedback, as in, ‘Wow, I can feel that breach!’”
Can’t Elongate the Day, But…
“As we continue to move into advanced training techniques and improve our surgical education in all fields, including synthetic models, augmented reality, virtual reality, etc., we must continue to advance surgical training outside the OR. The number of hours in the days are not increasing, so we need to find ways to improve the efficiency of our surgical training.”
“Not only have we here at Cedars Sinai benefitted from using these synthetic models in training simulations, which I think is correlated to improved surgical experience, but it has also improved surgical safety because trainees can practice on very realistic complex pathology prior to going into the OR. As someone who has to sit across from a trainee while he or she operates on young children, having these models is something that makes me very excited. Overall, I cannot say enough about how SurgiSTUD is allowing me to help trainees help patients.”
Hands-on Hips
Keith Berend, M.D. is an orthopedic hip and knee surgeon with JIS Orthopedics in Columbus, Ohio. “We had the privilege of working with the SurgiSTUD anterior hip models when we had the Rothman-Ranawat Hip Society visiting fellows at our facility. We spent an entire day in the lab with fresh human tissue (cadavers) using various approaches, techniques, new implant designs, and technologies like augmented reality and virtual reality. We literally went from using fresh human tissue to using SurgiSTUD for the same type of procedures with anterior hips and were able to compare the two hands-on within moments of each other. The fellows were incredibly impressed with the power of the SurgiSTUD concept.”

Wowed by the anatomical accuracy and reproducibility, the fellows also appreciated the natural feel that the SurgiSTUD models provide, says Dr. Berend. “Such qualities are vital, especially for fellows who aren’t very skilled in anterior hip surgery. All of this launched an in-depth conversation among our visiting fellows, myself, and my partners.”
“Once you are a resident or fellow you no longer need to learn anatomy—it’s surgical technique, tools, instruments, technology, and deformity—things that cadavers really can’t reliably allow you to learn. With SurgiSTUD, you can reproduce numerous variables accurately every single time and be able to use things like augmented reality. With SurgiSTUD you can dock, ream, broach and put in whatever deformity you want—no human tissue needed.”
Need to Know
“Honestly,” says Dr. Berend, surgeons who don’t know about SurgiSTUD don’t know what they don’t know. I will never bring in another cadaver. There are numerous, longstanding complaints that we all have regarding cadavers. Because of this, and the fact that SurgiSTUD works exquisitely well, I don’t think it’s going to be hard to break tradition.”
“Learning on a cadaver that is in no way similar to what I’m going to be doing in the OR is a waste of my time. Frankly, cadaver training probably isn’t as safe as we’ve considered it to be throughout the years.”
A new gold standard?
“I don’t think anything is going to outperform SurgiSTUD,” states Dr. Berend. “Patient-specific case-by-case training is going to have massive benefits for surgeons and patients alike. In addition, having a library of cases, deformities, conditions, and situations that surgeons can order from is invaluable. I can say, ‘I need a real bad Crowe IV dysplasia of a right hip…ok!’ and get exactly that.”
“Yes,” sums up Dr. Berend. “SurgiSTUD should be the gold standard for orthopedic training.”